The intercellular matrix makes up a significant part of the human body. Many tissues are only 20% cells and 80% matrix. The highest content of the matrix is observed in connective tissues: skin, bones, cartilage, tendons, blood, lymph, the iris and sclera of the eye, as well as in fascia - "cases" for muscles, organs, vessels and nerves.
The matrix has more than just a structural function. It is constantly in contact with cells through receptors on their surfaces. Such contact is critically important for the cell, since in its absence it commits a programmed death—apoptosis. The extracellular matrix also facilitates cell movement and migration. For example, it is the signals of the matrix that determine that the young stem cell is separated from the niche and migrates into the tissue, where it will need to turn into one or another type of specialized cells.
In general, the functions of the extracellular matrix include providing support for cells, separating tissues from each other, and regulating intercellular communication. It determines the dynamic behavior of cells, allocates a number of growth factors and acts as their “storage”, providing fast and directed tissue growth, for example, in the case of wounds and fibrosis. Understanding the structure of the extracellular matrix is important for effective diagnosis and treatment of cancer, since metastasis is often accompanied by the destruction of the matrix by specific enzymes, as well as the loss of the ability of cells to respond to its signals.
What is the extracellular matrix made of?
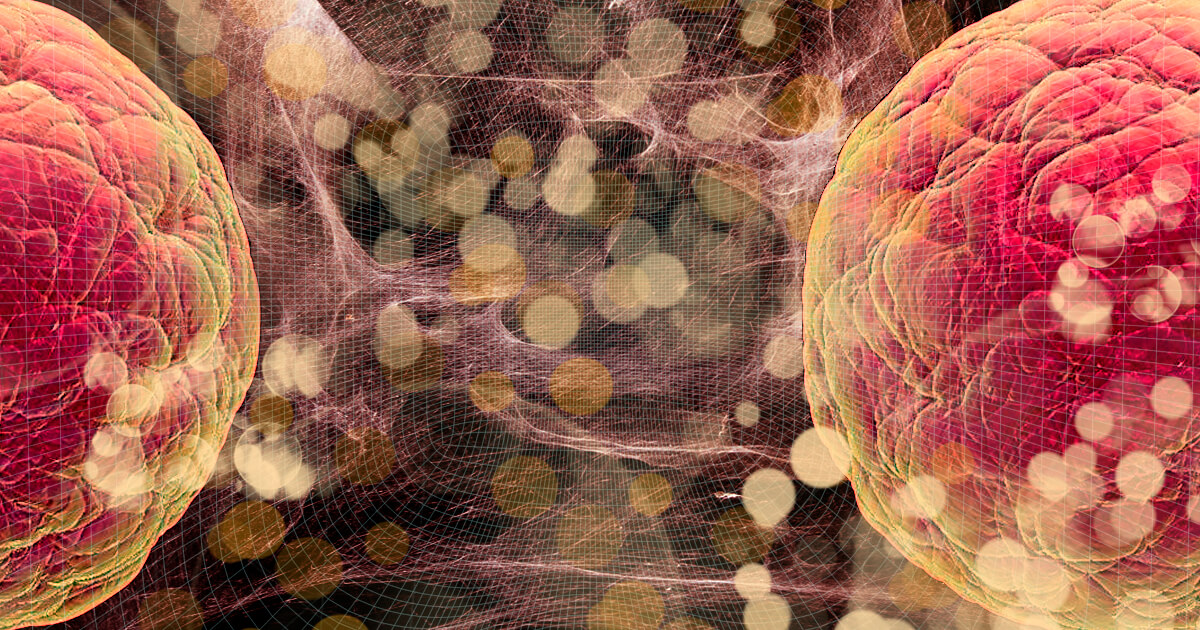
The matrix is a web-like structure between cells, which consists of elongated, long-lived molecules and "filler" between them.The structural function in the matrix is performed by special proteins: glycoproteins, elastic and reticular fibers. In the matrix, they can be compared to mattress springs. Glycoproteins consist of protein and an oligosaccharide chain, and their proportion of carbohydrates does not exceed 20%. The most common glycoproteins are collagen and elastin.
The main substance of the matrix is proteoglycans, hyaluronic acid and water molecules, which they retain. The matrix fills the space between structural proteins. Proteoglycans, like glycoproteins, consist of proteins and carbohydrates, but in the case of proteoglycans, the carbohydrate content reaches 90-95%. They work as a “warehouse” in which substances necessary for cells are stored.
The so-called adhesive glycoproteins are responsible for organizing the matrix into a “network”: laminin, fibrillin and fibronectin. They act as "glue" for the building blocks of the matrix and cells. For example, fibronectins bind cells to collagen fibers, allowing cells to move through the matrix. And the laminins are included to form networks that provide elasticity to the tissues.
The matrix containsgrowth factors—proteins that switch the cell mode into the division phase for regeneration. The matrix also includes enzymes - proteins that accelerate all reactions in cells: the synthesis of new substances and their breakdown. Most of the matrix is metalloproteinases—special enzymes that are able to break down the old matrix, which plays a critical role in its renewal.
Specialized cells are responsible for the synthesis of the extracellular matrix. In connective tissue, these are usually fibroblasts. They constantly produce and secrete matrix molecules into the surrounding space, which ensures its timely renewal. Fibroblasts are factories for renewing the extracellular matrix—this is their main function. However, other cells can also play the role of matrix creators. For example, chondrocytes are responsible for the formation of the matrix in cartilage, while osteoblasts are responsible for the formation of the matrix in the bones.
Collagen fibers
Collagen is the main structural protein in the matrix. It accounts for 25-33% of all proteins in the body. In the dermis of the skin, the collagen content reaches 70-80%, and in the bone tissue, more than 90%. Collagen is also found in cartilage, joints, hair, nails and even eyeballs. It is usually a long, thread-like molecule that is folded differently in different tissues. For example, in the skin, collagen forms a three-dimensional network of threads, and in the bones, the threads lie parallel, tightly pressed against each other.Depending on the degree of mineralization, collagen-rich tissues can be stiffer, like bone, or more elastic, like tendons. Often tissues are elastic at the beginning of life, but gradually mineralize. This, for example, happens with heart valves: with age, calcium is deposited in collagen, which impairs the work of the heart.
There are currently 28 types of collagen known. They differ from each other in the sequences of amino acids (the “building blocks” of which proteins are built), chemical modifications, and what structures they form. Collagens of types I, II, III, V, XI form long filaments, type IV forms films, and type VII - short filaments that act as “anchors”. Other collagens can also form short chains and spirals. More than 90% of all human collagen is in I (the strongest) and II, III and IV types.
Collagens are composed of amino acids, which are packed into filaments (fibrils) with a diameter of 1.5 nm and a length of about 300 nm. Fibrils, upon closer inspection, are helices of three strands: two identical (alpha peptide-1) and one slightly chemically different (alpha peptide-2). Fibrils, in turn, form bundles - these are collagen fibers.

Figure 1. Structure of type I collagen. Red line - collagen I-alpha-I, blue line - collagen I-alpha-II.
Each of the three chains of collagen fiber is initially synthesized separately, and then they are assembled into one spiral inside the fibroblast. At this stage, the coil is water soluble and called procollagen. The fibroblast then releases protocollagen into the extracellular environment, where it loses its solubility and organizes into extended fibers that form a three-dimensional network.
In the matrix, specific enzymes form cross-links between the collagen triple helix chains, as well as between different chains, which allows them to form fibrils. It is important to note that a small amount of cross-linking formed by enzymes is required for the formation of collagen fibers. However, the excess cross-linking that occurs with age is one of the factors of matrix aging.
Elastic fibers
The most important component of the extracellular matrix is elastic fibers, consisting of the protein elastin. These fibers are able to stretch in length for a distance many times their length, and then return to their original state. However, with age, the elasticity of these fibers decreases significantly.Elastin is insoluble, highly stable, and slowly metabolized. Most proteinases are unable to break it down. Only the enzyme elastase, which cells synthesize in the foci of inflammation, can cope with this.
Elastin is easily destroyed by direct sunlight - this explains the rapid aging of the skin and the loss of its elasticity in people who neglect sunscreens.
Elastin fibers are formed similarly to collagen fibers: first, chains of tropoelastin, the precursor of elastin, are assembled in fibroblasts. It is still a soluble molecule. After entering the matrix, crosslinks are formed in elastin with the help of specific enzymes, which stabilize the molecule.
The amorphous elastin network then combines with fibrillin-1a, a glycoprotein that acts as a “glue” in the matrix.
As a result, elastin fibers 1–2 µm thick are formed. The fibers branch out and connect to each other to form a network. The resulting fibers are elastic, resistant to the action of acids and alkalis, and do not swell in water. They are able to maintain their function throughout their lives. However, various enzymes such as matrix metalloproteinases and serine proteases can degrade them.
The main substance, or where is the injection of beauty
The main matrix filling substance consists of a large number of non-protein molecules. These are, first of all, various types of glycosaminoglycans—large polysaccharides that create mechanical support for cells. They bind water and fill the spaces between cells like a “gel”. The most common are dermatan sulfate, heparan sulfate, heparin, chondroitin sulfate, keratan sulfate, and hyaluronic acid.Most glycosaminoglycans, with the exception of hyaluronic acid, form proteoglycans. These are complex molecules, shaped like a dishwashing brush, where the axis is protein, and there are many "fibers" of carbohydrates around. Moreover, the protein part is only 5-10% of the mass of the molecule, and the remaining 90-95% are "villi". These "brushes" are attached to the hyaluronic acid thread. The result is a centipede with "brush" legs.
Water molecules, ions, signaling molecules, and growth factors are retained in these proteoglycan “brushes”. This allows the matrix to act as a tissue “depot” of regulatory substances. In addition, proteoglycans coat the cell surface and play an important role in ion exchange, immune responses, and tissue differentiation.
The most biologically active glycosaminoglycan is heparan sulfate. It determines whether the cell will divide or migrate, participates in the formation of collagen fibers and wound regeneration. Thanks to heparan sulfate, cells can attach to matrix proteins, which allows them to receive signals from their environment. Disruption of this interaction occurs with age and can lead to inflammation.
Dermatan sulfate is a major constituent of the skin's basic substance and is also found in blood vessels, heart valves, tendons, and lungs. In addition to performing a structural function, it plays a role in coagulation (blood clotting), pathogenesis of cardiovascular diseases, carcinogenesis, infectious processes, wound healing and fibrosis.
One of the most important non-protein components of the extracellular matrix is hyaluronic acid. From a chemical point of view, it is a polymer consisting of D-glucuronic acid and D-N-acetylglucosamine residues. It performs a number of functions essential for the matrix: it stabilizes collagen fibers, participates in the interaction and migration of cells, and plays an important role in wound healing.
The most remarkable property of hyaluronic acid is moisture retention: one hyaluronan molecule is able to capture and hold 500 water molecules around it. this liquid is then used for hydration, cellular interactions or to create tissue volume. It is the last property that cosmetologists use when injecting hyaluronic acid, for example, into the lips. The gel-like substance will "swell" with any moisture and maintain its volume, which explains the effect of cosmetic procedures.
Hyaluronic acid is synthesized mainly by fibroblasts of the dermis of the skin and is rapidly renewed: about a third of all hyaluronic acid per day. It is curious that it is hyaluronic acid that determines the extreme longevity of naked mole rats - animals with negligible aging. Naked mole rat hyaluronic acid molecules have a higher molecular weight, which suppresses inflammation and cell division, preventing the development of cancer.
Matrix update
The components of the matrix are constantly updated: the old ones are cleaved by matrix metalloproteinases, and the new ones are synthesized by specialized cells (for example, fibroblasts). Renewal occurs most intensively after injuries and burns. Some components of the matrix are updated quickly. Others, like collagen and elastin, are amazingly long-lived. The half-life of collagen in cartilage is as much as 95 years. During this time, a number of damages accumulate in the collagen, which greatly contributes to the aging of the matrix.Communication of the matrix with the cell
The matrix performs not only a structural, but also a communicative function. The main place here is occupied by selectins—glycoproteins that penetrate the cell membrane and participate in the binding of the cell to the matrix and other cells. They are involved in intracellular signaling, as well as in the recruitment and migration of leukocytes to sites of inflammation. Increased activation of selectins can occur with the development of age-related pathological processes, for example, with atherosclerosis, deep vein thrombosis, and the start of metastasis in tumors.Thus, the extracellular matrix is a dynamic extracellular component of the body. It is responsible for regulating cell division, survival, differentiation, and migration. It constantly undergoes remodeling in response to various stimuli and changes significantly during the aging of the body.